Cervical cancer is the fourth most common cancer in women globally..Despite being preventable and treatable, it continues to devastate the lives of several women each year. burden of cervical cancer is particularly heavy in low- and middle-income countries where about 85% of cases occur .
In 2020, there were an estimated 604,127 cases and 341,831 deaths attributed to cervical cancer. It is estimated that the cases increased to 7,00,00 and 4,00,000 deaths estimated by 2030
It is second most common cancer in india.The estimated number of cervical cancer cases in India in 2023 is over 3.4 lakh.60% of cases detected in an advanced stage.60,000 women die of cervical cancer every year
The adverse impacts of cervical cancer extend beyond health. They affect the social and economic fabric of families and communities. Women, who are often the backbone of their families, face not only physical suffering but also emotional and financial strain. Many women diagnosed with cervical cancer are in their prime years, which means their illness and potential loss affects the stability and prosperity of entire families.
Causes of cervical cancer

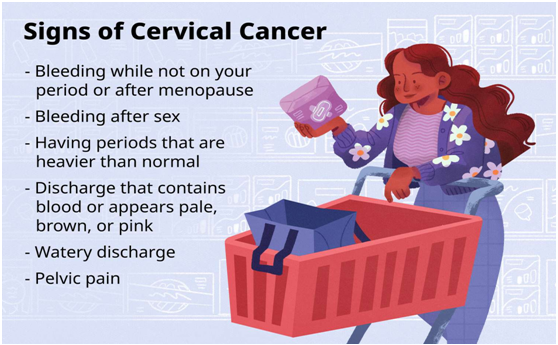
Cervical cancer is caused primarily by the Human Papillomavirus (HPV), a sexually transmitted infection. Apart from HPV other Sexually Transmited diseases are also known to cause cervical cancer.
Second most important contributing factor is low immunity. females with immune compromised conditions like HIV,patients receiving drugs which lower the immunity are at risk of developing cervical cancer.
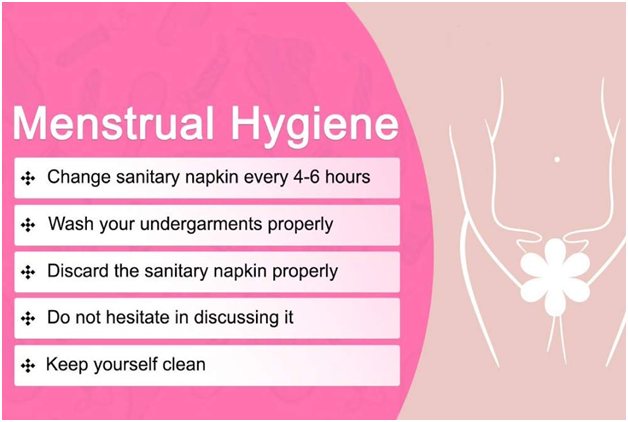
Lack of personal hygiene and Smoking also contribute to cervical cancer
Cervical cancer elimination
The World Health Organization (WHO) has taken cervical cancer elimination as a global movement since 2020.
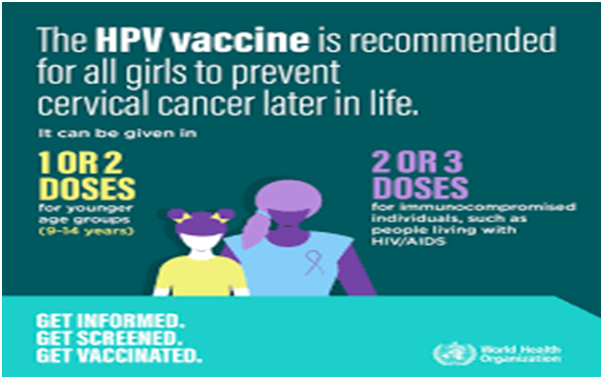
WHO has launched a global strategy to eliminate cervical cancer as a public health problem. This strategy outlines a comprehensive approach, focusing on three key pillars: vaccination, screening, and treatment.
90–70–90 targets that must be met by 2030
90% of girls fully vaccinated with HPV vaccine by age 15 years
70% of women are screened with a high-performance test by 35 years of age and again by 45 years of age
90% of women identified with cervical disease receive treatment (90% of women with pre cancer treated, and 90% of women with invasive cancer managed)
Associate countries agreed to reach the targets by 2030
Prevention
Cervical cancer can be prevented by Screening, vaccination and personal hygiene
Main challenge of cervical cancer screening is stigma, lack of awareness and limited access to health care facilities
Cervical cancer screening Guidelines:-
Screening starts from age of 21.
Between 21-29-pap smear every 3 years
29-65-pap smear every 3 years or
pap smear plus HPV test once in 5 years